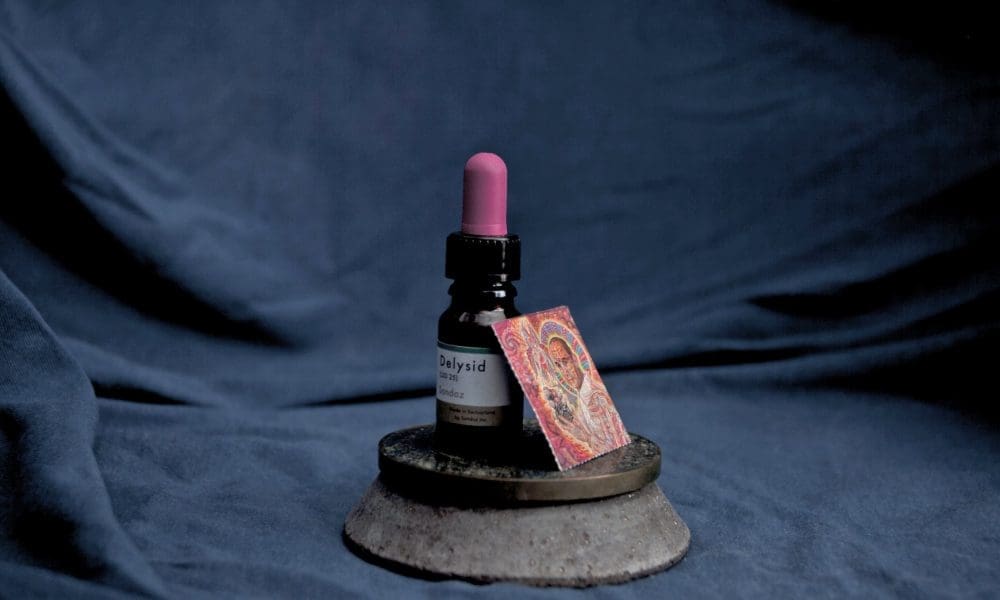
LSD-Like Drug Wins FDA ‘Breakthrough Therapy’ Status For Treatment Of Generalized Anxiety Disorder
Science & Health Archives – Marijuana Moment Read More [[{“value”:” Promising results from a clinical trial of the LSD-like substance MM120 have persuaded the Food and Drug Administration (FDA) to award it “breakthrough therapy” status as a treatment for generalized anxiety disorder (GAD). The drugmaker behind MM120—Mind Medicine Inc., or MindMed—said in a press release […]