Marijuana Study Comparing U.S. And Canada Finds Broad Legalization Support And Similar Use Rates Despite Differing National Policies
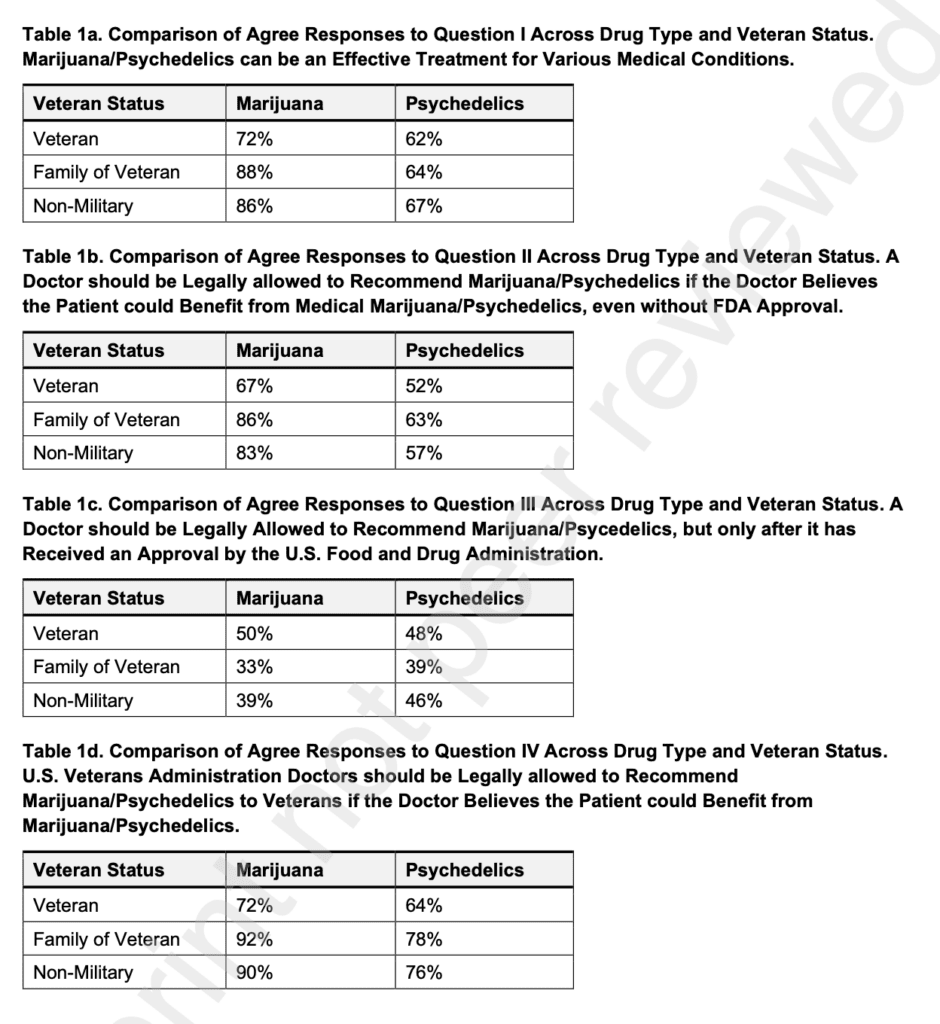
Science & Health Archives – Marijuana Moment Read More A new survey published in the Journal of Cannabis Research found strong majority support for legal cannabis among respondents from both the United States and Canada, along with just under half of people in both countries saying that they consume cannabis. The trends were overall very […]